Claim Processing
MetLife’s goal is to settle your claims as quickly and accurately as possible.

For some complex procedures, our claim consultants may require additional information from your dentist, meaning the claim takes a little longer to process.
Claim processing from start to finish
It’s important to understand the steps involved in processing and paying claims. Below is a typical sequence of events involved in processing a claim.
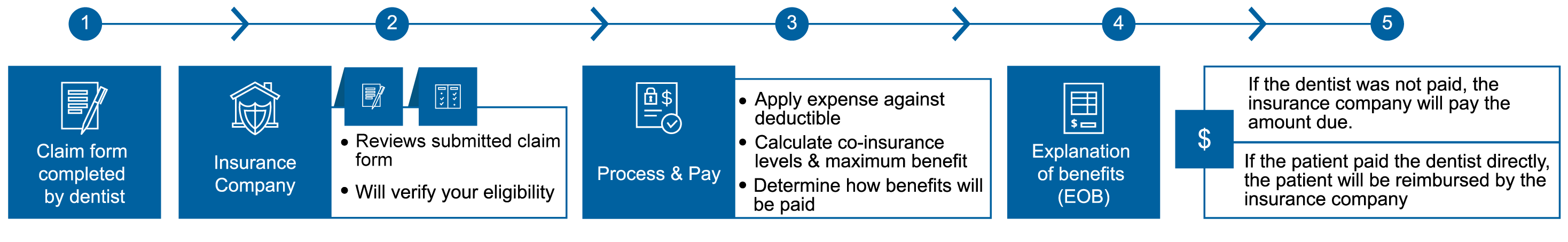
- Dental offices will usually complete the claim form and submit it to your insurance company.
- The insurance companies receives the completed claim form and verifies your eligibility.
- Your treatment is compared with your dental plan to determine covered expenses and non-covered expenses. Covered expenses are applied against your deductible, co-insurance levels and the maximum benefit to determine how benefits should be paid.
- Claim is processed. An Explanation of Benefits (EOB) statement is created and sent to you. This explains how much was paid as a benefit and how much you are responsible for.
- Payment is issued. This is usually paid to your dentist but will go directly to you if you paid your dentist in full for the treatment at time of service.
Checking the status of a claim
You can track your claims online and receive an e-mail alert once a claim has been processed.
Call 1-800-942-0854
(You can access MetLife’s automated voice response system 24 hours a day, 7 days a week.*)
*Except when our systems are undergoing scheduled maintenance or unscheduled interruption.